FACT SHEET: Hypertension in Adults (also known as “high blood pressure” or “high BP”)
Note: This fact sheet focuses on hypertension in persons aged 18 years and older. For hypertension in children (i.e., persons aged less than 18 years), refer to Hypertension in Children & Adolescents Fact Sheet.
Is the initiation of non-invasive dental hygiene procedures* contra-indicated?
- No, unless systolic blood pressure (SBP) ≥ 180 mm Hg and/or diastolic blood pressure (DBP) ≥ 110 mm Hg OR there are warning symptoms/signs in the hypertensive patient/client at lower levels of BP; e.g., severe headache, blurred vision, shortness of breath, nosebleeds, nausea/vomiting, chest pain, or seizures. (See attached tables for further details.)
Is medical consult advised?
- Yes, if SBP > 130 mm Hg and/or DBP > 85 mm Hg1; in patients/clients with diabetes, medical consult is advised at DBP > 80 mm Hg.
Is the initiation of invasive dental hygiene procedures contra-indicated?**
- No, unless SBP ≥ 180 mm Hg and/or DBP ≥ 110 mm Hg OR there are warning symptoms/signs in the hypertensive patient/client at lower levels of BP; e.g., severe headache, blurred vision, shortness of breath, nosebleeds, nausea/vomiting, chest pain, or seizures. In patients/clients with risk factors such as myocardial infarction, angina pectoris, high coronary disease risk, recurrent stroke, diabetes mellitus, and renal disease, invasive procedures should not be performed if SBP ≥ 160 mm Hg and/or DBP ≥ 100 mm Hg. (See attached tables for further details.)
Is medical consult advised?
- See above.
Is medical clearance required?
- No.
Is antibiotic prophylaxis required?
- No.
Is postponing treatment advised?
- No, unless BP is at contra-indication levels (see above) or there are other concerns that invasive procedures may significantly elevate patient/client blood pressure (e.g., missed anti-hypertensive medications), which should prompt medical consultation prior to the performing of invasive procedures. Dental hygiene procedures should be deferred for any patient/client who has uncontrolled hypertension (BP of 180/110 mm Hg or higher in persons without a history of other cardiovascular risk factors; 160/100 mm Hg or higher with a history of other risk factors). Asymptomatic patients/clients with BP less than 180/110 mm Hg (or 160/100 in patients/clients with other cardiovascular risk factors) can receive any indicated dental hygiene treatment; however, persons with elevated blood pressures (particularly 135/85 AOBP2 or 140/90 OBPM3 or non-AOBP4 and higher in most people) should be encouraged to see their physician for investigation and optimal management, as per attached tables).
Oral management implications
- Automated (electronic, oscillometric5) blood pressure measurement is preferred over manual and auscultatory measurement in adults.
- The primary concern in dental hygiene management of a patient/client with hypertension is that during the course of treatment a sudden, acute elevation of blood pressure might occur, potentially leading to a serious outcome, such as heart attack or stroke. Emotional stress and pain stimulate the sympathetic nervous system, which can result in elevated blood pressure. The two important questions to be answered before dental hygiene treatment are: 1/ what are the associated risks of treatment in this patient/client; and 2/ at what level of blood pressure is treatment unsafe for the patient/client.
- The procedural risk associated with an adverse cardiovascular outcome from both non-invasive and invasive dental hygiene procedures is very low. The risk imposed by uncontrolled blood pressure (defined as 180/110 or greater in most persons) constitutes a minor risk in terms of dental hygiene cardiovascular risk; however, blood pressure should be brought under control before elective procedures or surgery are performed.
- In general, short morning appointments seem best tolerated in patients/clients with hypertension.6 Stress management is important to decrease the chances of endogenous release of catecholamines that might increase blood pressure.
- Orthostatic hypotension (i.e., low blood pressure when standing erect) can result from drugs (e.g., alpha-adrenergic blockers, angiotensin converting enzyme inhibitors, angiotensin II receptor blockers, and direct vasodilators) used to treat hypertension. Dental hygienists can minimize patient/client light-headedness or fainting by avoiding rapid chair position changes.
- Alpha-adrenergic blockers can result in nasal congestion, which should be considered where nasal breathing is relied upon.
- Beta-blockers can result in dizziness, bronchospasm, and masking of hypoglycemia; the dental hygienist should be alert to these possible drug side effects.
- Dental hygienists should educate patients/clients when abnormal vital signs (including blood pressure) are present, and recommend medical referral when appropriate. They should encourage compliance with recommended physician hypertension management plan, including prescription medications.
- Dental hygienists should counsel patients/clients who smoke (particularly those who are hypertensive) to stop smoking and refer them to cessation supports in their local communities (e.g., public health unit, smokers’ help line, etc.). In Ontario, the Canadian Cancer Society offers a free, confidential Smokers’ Helpline for smokers via Telehealth Ontario at 1‑866‑797‑0000 or 1-877-513-5333; Smokers’ Helpline Online is available at www.smokershelpline.ca.
Oral manifestations
- None are specific to hypertension, but the contributory factor smoking has well-known oral manifestations. The development of facial palsy has been described in the occasional patient/client with very severe hypertension. Excessive bleeding after surgical procedures or trauma has been uncommonly reported in patients/clients with severe hypertension.
- Side-effects of anti-hypertensive medications include:
- chronic cough (e.g., angiotensin converting enzyme inhibitors — ACEIs), as well as direct renin inhibitors);
- taste changes (e.g., ACEIs, beta blockers, alpha-adrenergic blockers, and calcium channel blockers — CCBs);
- loss of taste (e.g., ACEIs and angiotensin II receptor blockers — ARBs);
- angioedema of lips, face, tongue (ACEIs and ARBs);
- upper respiratory tract infections (e.g., ARBs);
- gingival hyperplasia/overgrowth (e.g., CCBs);
- dry mouth (e.g., thiazide diuretics and alpha-adrenergic blockers);
- lichenoid reactions7 (e.g., thiazide diuretics and beta blockers);
- lupus-like oral and skin lesions (e.g., direct vasodilators); and
- parotid pain (e.g., central alpha-adrenergic — alpha 2 — agonists).
Related signs and symptoms
- Hypertension (HTN) is typically a persistent or repeatedly elevated AOBP ≥ 135/85 mm Hg OR non-AOBP ≥ 140/90 or ≥ 130/80 in patients/clients with diabetes.8 [Note: If dedicated office visit #1 to a qualified healthcare professional reveals mean AOBP or non-AOBP SBP ≥ 180 mm Hg and/or DBP ≥ 110 mm Hg, then hypertension is automatically diagnosed.]
- Hypertension affects about one in five Canadian adults, and its incidence increases with aging. If people live long enough, more than 90% will develop hypertension.
- Only 72% of affected Canadian adults are treated for hypertension, and only 58% are adequately controlled.
- The relationship between blood pressure (BP) and risk of cardiovascular disease (CVD) is independent of other risk factors; the higher the BP, the greater the likelihood of myocardial infarction (heart attack), heart failure, stroke, and kidney disease. Other examples of end organ damage include peripheral artery disease (e.g., intermittent claudication) and retinal damage (which may lead to loss of vision).
- About 90% of hypertension is primary (also known as “essential” or “idiopathic”; i.e., no readily identifiable cause). Up to 10% is secondary (e.g., caused by an identifiable underlying cause, such as renal insufficiency, renovascular disease, primary aldosteronism, aortic coarctation, Cushing’s syndrome, Conn’s syndrome, or pheochromocytoma). Drug-induced hypertension and white coat hypertension (i.e., elevated BP only in the presence of a health care worker) are other causes of elevated blood pressure.
- The following coexisting conditions may contribute to hypertension: alcohol intake (more than one standard drink per day); anxiety disorders; delirium; hyperinsulism with insulin resistance; obesity; pain (acute or chronic); pregnancy; sleep apnea; and smoking.
- Many medications are used to treat hypertension resistant to lifestyle changes. More than 40% of Canadians aged 60 years or over are on antihypertensive therapy. Dental hygienists are most likely to encounter patients/clients taking thiazide diuretics (e.g., hydrochlorothiazide,) or thiazide-like diuretics (diuretics often being referred to as “water pills” by patients/clients); beta-blockers (e.g., atenolol); angiotensin converting enzyme inhibitors (ACEIs, such as ramipril); angiotensin II receptor blockers (ARBs, such as losartan); and various long-acting calcium channel blockers (CCBs, such as felodipine, diltiazem, and verapamil). Less frequently used are direct renin inhibitors (e.g., aliskiren fumarate), alpha-adrenergic blockers (e.g., terazosin), and direct vasodilators (e.g., hydralazine).
The tables that follow are intended only as guides to help inform decision-making. The dental hygienist must also consider the current clinical status of the patient/client in the office. Patients/clients with high blood pressure who have signs/symptoms such as severe headache, blurred vision, shortness of breath, nosebleeds, nausea/vomiting, chest pain, or seizures, should be referred to a physician for immediate evaluation. Furthermore, the dental hygienist should compare current BP reading with previous readings. A person who typically has low or normal blood pressure who now has unexpectedly elevated blood pressure may be more worrisome in the short-term than a person who habitually has high blood pressure.
Where the tables advise that non-invasive procedures (e.g., oral hygiene instruction, fitting a mouth guard, and taking an impression) +/- invasive procedures (i.e., scaling teeth and root planing, including curetting surrounding tissue) may be undertaken, the dental hygienist should consider the individual circumstances of each patient/client. Specific procedures (be they non-invasive or invasive) should be avoided if the dental hygienist believes they could cause stress/anxiety resulting in a sudden, acute elevation in blood pressure. This individual consideration of stress/anxiety is particularly important for patients/clients with pre-existing high blood pressure. If in doubt, the dental hygienist should defer the procedure(s) pending medical evaluation.
CDHO Advice for Adults Incorporating Hypertension Canada/CHEP Recommendations and Oral Health‑Specific Sources
Table 1 ****This table is to be used if an adult patient/client presents WITHOUT A HISTORY of other risk factors such as history of myocardial infarction, angina pectoris, high coronary disease risk, recurrent stroke, diabetes mellitus, or renal disease.
Note: AOBP = automated office blood pressure; non-AOBP = non-automated office blood pressure (BP readings in Table 1 refer to non-AOBP unless otherwise indicated.)
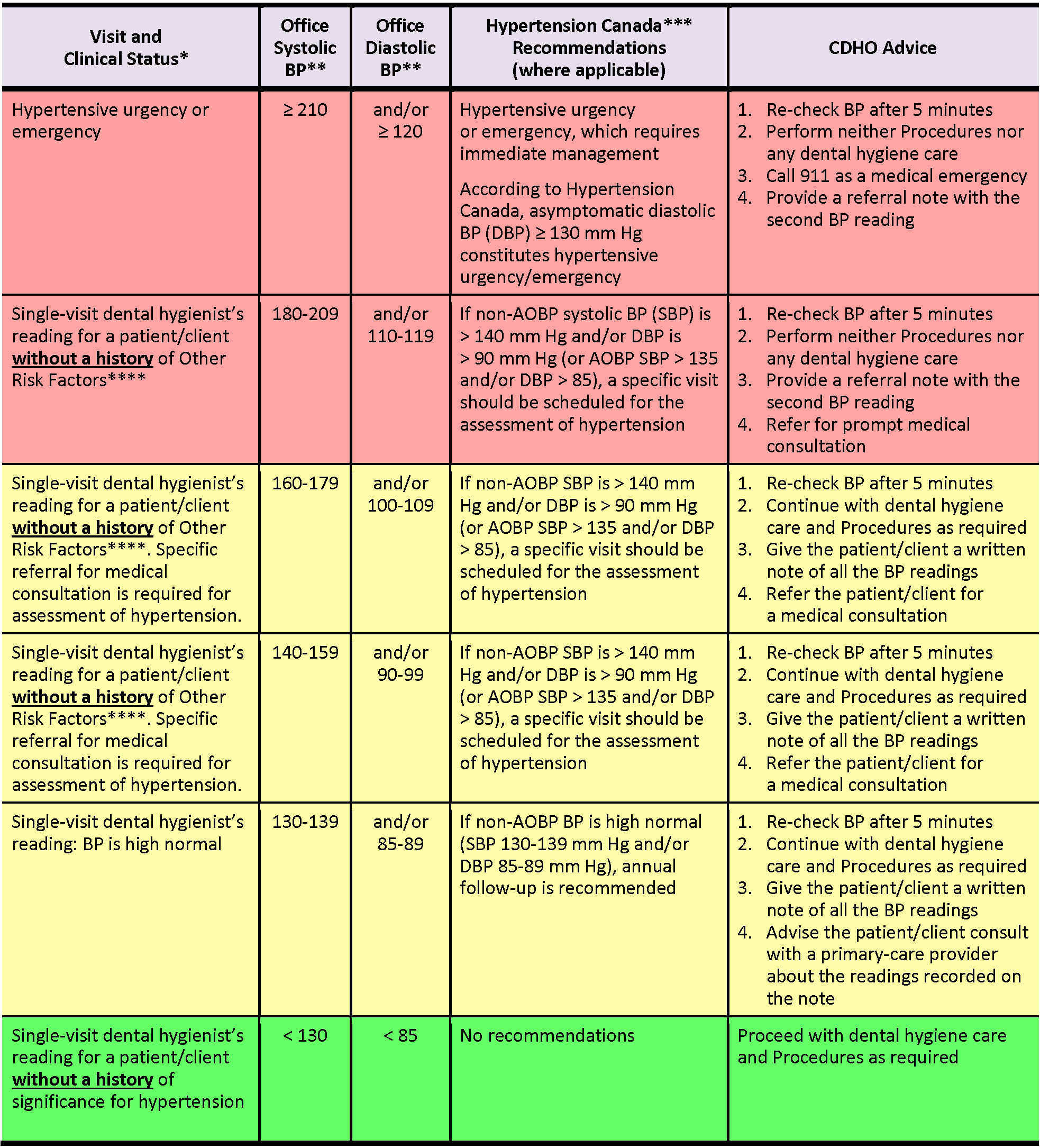
Table 2 ****This table is to be used if an adult patient/client presents WITH A HISTORY of risk factors such as history of myocardial infarction, angina pectoris, high coronary disease risk, recurrent stroke, diabetes mellitus, or renal disease.
Note: AOBP = automated office blood pressure; non-AOBP = non-automated office blood pressure (BP readings in Table 2 refer to non-AOBP unless otherwise indicated.)
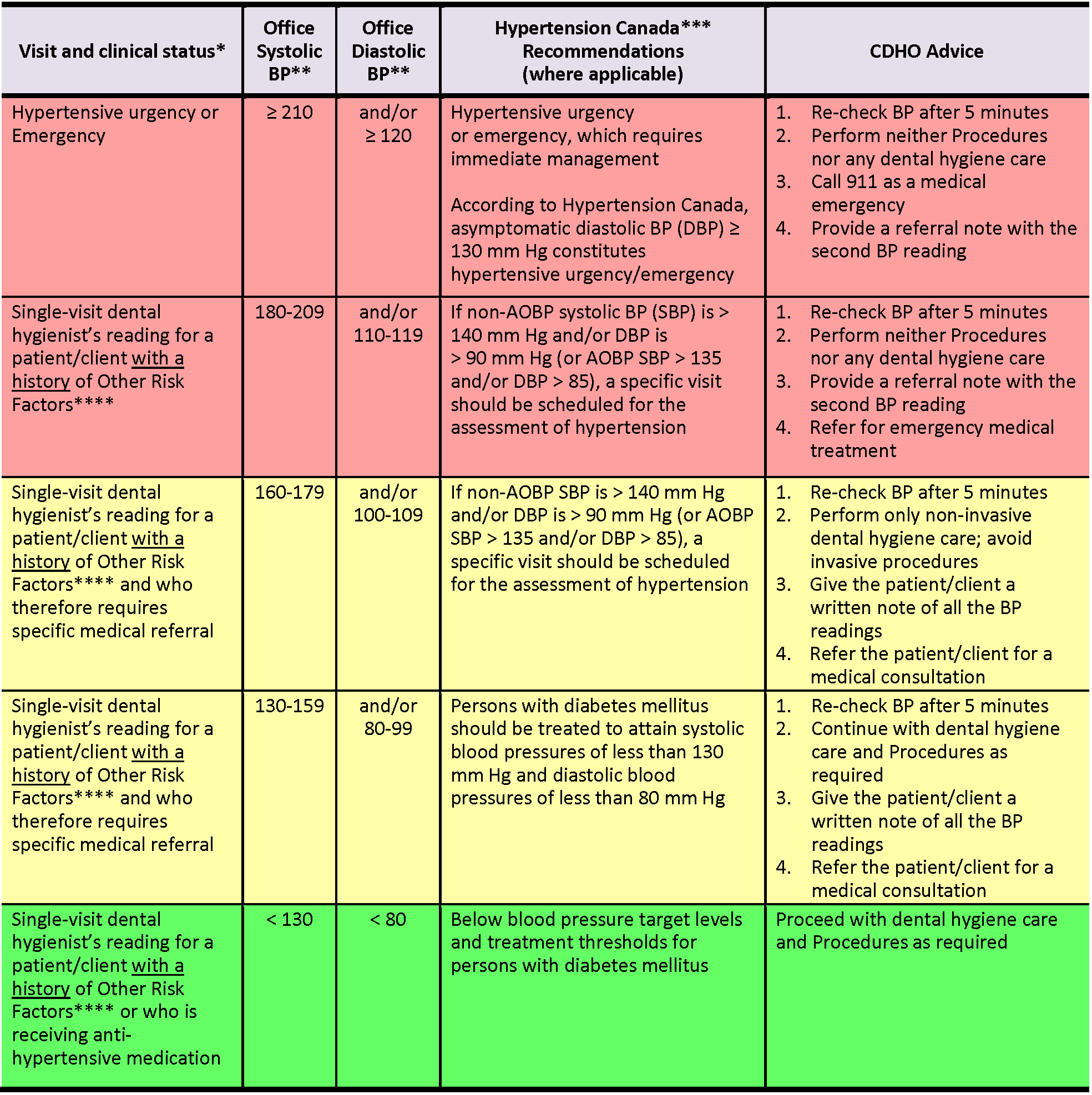
* Assumes that the measurement is repeated at least once over a period of five minutes or more, with the patient/client at rest
** mm Hg (≥ means ‘equal to or more than’; < means ‘less than’; ≤ means ‘equal to or less than’)
*** CHEP 2016 Guidelines stated that target systolic BP in the very elderly (age ≥ 80 years) is < 150 mm Hg, rather than < 140 mm Hg in other, non-diabetic adults. However, superseding this, Hypertension Canada’s 2017 Guidelines (formerly CHEP Guidelines) stated that target systolic BP is ≤ 120 mm Hg for high-risk patients/clients, which includes persons age ≥ 75 years.
**** Other Risk Factors: history of myocardial infarction, angina pectoris, high coronary disease risk, recurrent stroke, diabetes mellitus, renal disease
References and sources of more detailed information
- College of Dental Hygienists of Ontario
https://cdho.org/advisories/hypertension/
https://cdho.org/factsheets/hypertension-in-children-adolescents/ - Leung AA, Bell A, Tsuyuki RT, Campbell NRC. CMAJ. 2021 Jun;193(23):E854-E855. DOI:10.1503/cmaj.210140. https://www.cmaj.ca/content/193/23/E854
- Zahedi S and Marciniak R. The Hypertensive Patient (A review of the latest Joint National Committee on Prevention, Detection, Evaluation and Treatment of Hypertension as it applies to the dentist). Oral Health 2012-02-01. https://www.oralhealthgroup.com/features/the-hypertensive-patient/
- Hypertension Canada https://guidelines.hypertension.ca/
- Hypertension Canada’s 2020-2022 Hypertension Highlights: A Practical Guide informed by the Hypertension Canada Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension
https://hypertension.ca/wp-content/uploads/2020/10/2020-22-HT-Guidelines-E-WEB_v3b.pdf - Hypertension Canada’s 2020 Hypertension Highlights: A Practical Guide informed by the Hypertension Guidelines for the Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension
https://hypertension.ca/wp-content/uploads/2018/07/Hypertension-Guidelines-English-2018-Web.pdf - Hypertension Canada’s 2020 Comprehensive Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults and Children
https://www.onlinecjc.ca/article/S0828-282X(20)30191-4/fulltext - Hypertension Canada’s 2018 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults and Children
https://www.onlinecjc.ca/article/S0828-282X(18)30183-1/fulltext - Hypertension Canada’s 2017 Guidelines for the Management of Hypertension
https://www.hypertension.ca/images/CHEP_2017/HTN_Whats_New_2017_EN.pdf - Hypertension Canada’s 2017 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults
http://www.onlinecjc.ca/article/S0828-282X(17)30110-1/pdf - Hypertension Canada’s May 2016 Hypertension in Canada Fact Sheet
https://hypertension.ca/wp-content/uploads/2018/12/HTN-Fact-Sheet-2016_FINAL.pdf - Canadian Hypertension Education Program’s 2016 Guidelines
https://www.onlinecjc.ca/article/S0828-282X(16)00192-6/fulltext - Government of Canada
https://www.canada.ca/en/public-health/services/chronic-diseases/cardiovascular-disease/hypertension.html - Heart & Stroke Foundation https://www.heartandstroke.ca/-/media/pdf-files/canada/health-information-catalogue/en-get-your-blood-pressure-under-control-v21-web.ashx?la=en&hash=20493566724F3F87387717A720D49F60521C1CF2
- American College of Cardiology/American Heart Association’s 2017 Hypertension Guidelines and related commentary
https://www.acc.org/latest-in-cardiology/articles/2019/04/04/12/50/similarities-and-differences-between-the-2017-acc-aha-bp-guideline-and-2017-ada-diabetes-and-htn-position-statement - American College of Cardiology/American Heart Association’s 2019 Guideline on the Prevention of Cardiovascular Disease
https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2019/03/07/16/00/2019-acc-aha-guideline-on-primary-prevention-gl-prevention - American Heart Association’s 2021 Scientific Statement on Management of Stage 1 Hypertension in Adults With a Low 10-Year Risk for Cardiovascular Disease: Filling a Guidance Gap
https://www.ahajournals.org/doi/full/10.1161/HYP.0000000000000195 - Centers for Disease Control and Prevention
https://www.cdc.gov/bloodpressure/ - American Dental Association
https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/hypertension - Bowen DM (ed.) and Pieren JA (ed.). Darby and Walsh Dental Hygiene: Theory and Practice (5th edition). St. Louis: Elsevier; 2020.
- Little JW, Falace DA, Miller CS and Rhodus NL. Dental Management of the Medically Compromised Patient (9th edition). St. Louis: Elsevier; 2018.
- Malamed SF. Medical Emergencies in the Dental Office (7th edition). St. Louis: Mosby Elsevier; 2015.
- Pickett FA and Gurenlian JR. Preventing Medical Emergencies: Use of the Medical History in Dental Practice (3rd edition). Baltimore: Wolters Kluwer Health, 2015.
FOOTNOTES
2 AOBP = automated office blood pressure (i.e., BP obtained via automated electronic upper arm device)
3 OBPM = office blood pressure measurement (i.e., BP obtained via an upper arm device with the provider in the room; oscillometric or electronic devices are preferred in adults, but auscultatory — mercury or aneroid — manual devices are an alternative)
4 Non-AOBP = non-automated office blood pressure (e.g., BP obtained via non-automated blood pressure cuff with provider in the room)
5 Oscillometric determination of blood pressure entails use of an automated device that measures mean arterial pressure. Systolic and diastolic blood pressure are then calculated via an algorithm.
6 Some authorities suggest that older patients/clients have their appointments in the late morning or early afternoon when their BP tends to be lower.
7 Lichenoid drug reactions/eruptions are also known as drug-induced lichen planus.
8 Hypertension Canada’s 2020 Guidelines also define home BP monitoring threshold for diagnosis as BP ≥ 135/85 mm Hg and ambulatory blood pressure monitoring (ABPM) threshold for diagnosis as a mean 24-hour BP ≥ 130/80 or a mean daytime BP ≥ 135/85. Hypertension Canada’s 2017 Guidelines (formerly the Guidelines of the Canadian Hypertension Education Program [CHEP]) removed age and frailty restrictions for the treatment of uncomplicated hypertension. In contrast to CHEP 2016 (which recommended target systolic BP in the very elderly [age ≥ 80 years] to be < 150 mm Hg), Hypertension Canada 2017 recommended office-setting systolic target of ≤ 120 mm Hg in high-risk patients/clients, which included persons age ≥ 75 years.
* Includes oral hygiene instruction, fitting a mouth guard, taking an impression, etc.
** Ontario Regulation 501/07 made under the Dental Hygiene Act, 1991. Invasive dental hygiene procedures are scaling teeth and root planing, including curetting surrounding tissue.
